 Hospital-based rehabilitation programs are expecting to see a major influx of medically complex patients, including those with neurological conditions, in the coming decades. However, COVID-19 has further spurred the drastic increase and caused an immediate rise in medically complex patients with multiple comorbidities.
Hospital-based rehabilitation programs are expecting to see a major influx of medically complex patients, including those with neurological conditions, in the coming decades. However, COVID-19 has further spurred the drastic increase and caused an immediate rise in medically complex patients with multiple comorbidities.
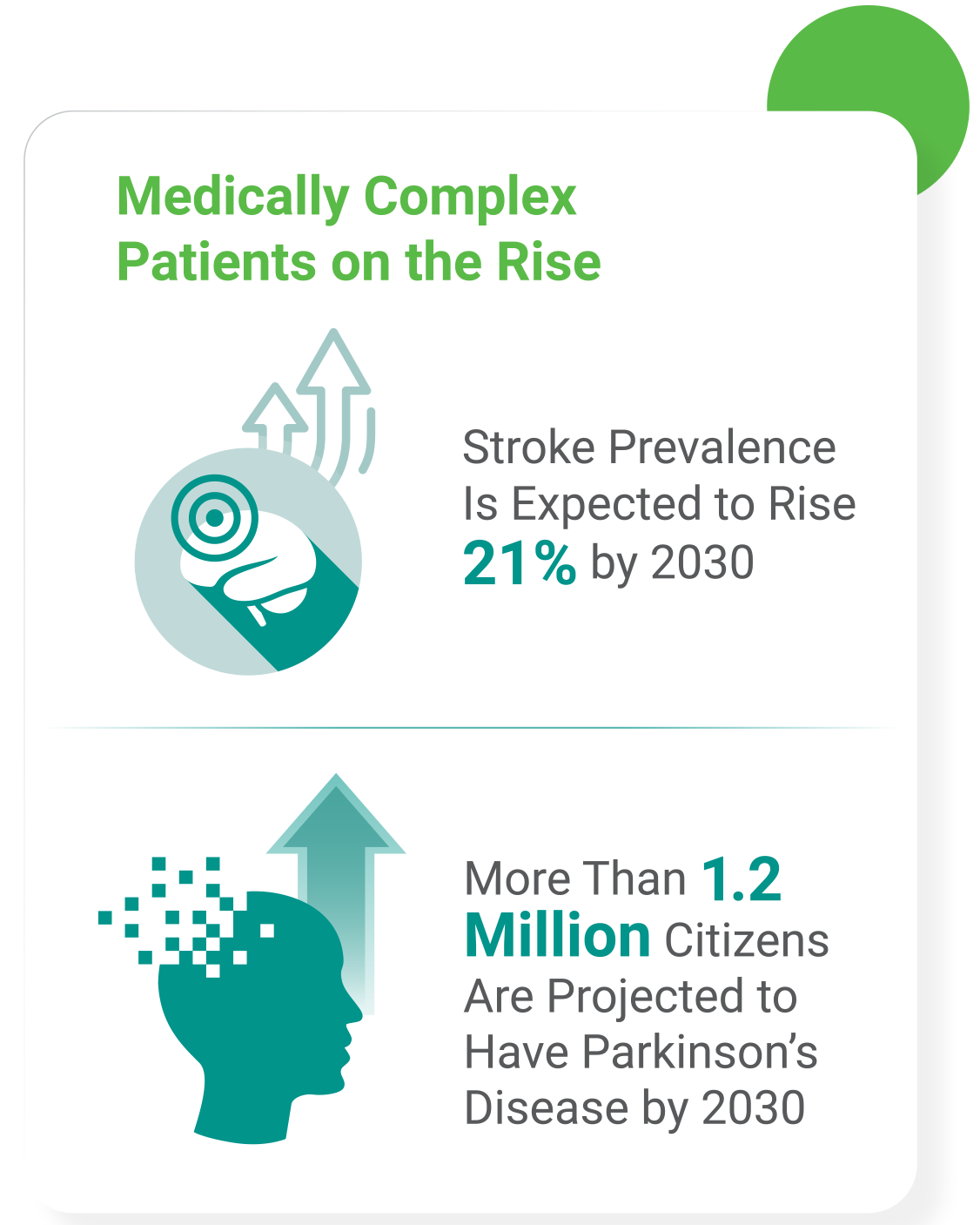
For example, stroke prevalence is expected to rise 21% by 2030, and more than 1.2 million citizens are projected to have Parkinson's disease.1,2 Moreover, patients experiencing prolonged symptoms of COVID-19, also known as long-haulers, are expected to face additional medical complexities and disabilities.3
This leaves hospital leaders with a significant question: What can be done to care for the current and future medically complex patient population, especially in a hospital rehabilitation setting? By efficiently and effectively evolving to meet the needs of this growing population, rehabilitation programs can successfully meet the challenge at hand, providing patients with the highest quality of care while achieving greater performance standards.
In this guide we'll examine the three areas that drive the greatest impact on treating medically complex patients:
1. Getting Your Staff Prepared Clinically
Many rehabilitation programs make the mistake of trying to serve this new medically complex patient population with the same staffing model that they have used in the past. Unless staffing models are quickly optimized for the new population, outdated staffing models can lead to operational inefficiencies and subpar outcomes. This need is further highlighted by recent studies that have found the first three months after discharge from COVID-19 treatment are the most critical to recognize and address emerging problems such as loss of function, cognitive impairment, pain, depression and more.4 Positions that are particularly important for treating medically complex patients are:
Rehab-Experienced Nurses
Unlike standard medical nurses, rehab-experienced nurses are trained to help patients with disabilities and chronic illnesses achieve maximum functional improvements. They pursue specialized certification through the Association of Rehabilitation Nurses which educates them to understand the treatments and systems used specifically in rehabilitation environments. This expertise translates to faster recovery for patients and more efficient programs.
Additionally, recent research uncovered that individuals discharged after experiencing severe cases of COVID-19 significantly benefited from multidisciplinary inpatient rehabilitation.5 This finding further supports inpatient rehabilitation's unique and vital role in a COVID-19 patient's recovery journey, as well as the importance surrounding the education and training for rehab-experienced nurses to help ensure patient outcomes and care quality standards are met.
Speech-Language Pathologists
Speech-language pathologists (SLPs) play an important role in helping patients reach optimal functionality. Throughout a patient's stay in a hospital, SLPs provide evaluations and treatment for swallowing disorders and speech and language problems resulting from strokes, head injury, respiratory issues and other medical complications.
This specialized form of care is proven vital. SLPs collaborate with physicians, nurses, other rehabilitation providers, dietitians, social workers and case managers to help ensure thorough education is provided about the patient's care status and effective treatment is given for optimal care.6 For instance, receiving speech therapy early in the rehabilitation process is most effective at treating aphasia, which is present in up to 38% of stroke patients.7 Research finds that more intensive therapy typically correlates with better outcomes.
Clinical Liaisons and Certifications
 A key part of optimizing the efficacy of your rehabilitation program is providing the right level of care at the right time. Highly-trained clinical liaisons are needed to achieve optimal timing of rehabilitation entry, in turn creating a positive patient experience, effective discharge planning and a reduced risk of readmission. CARF and Joint Commission certifications improve the comprehensiveness of patient treatment and the range of patients a program may treat, as well as help support improved program performance. On average, CARF accredited programs experience a 26% increase in annual patients served as well as a 37% increase in conformance to quality standards.8
A key part of optimizing the efficacy of your rehabilitation program is providing the right level of care at the right time. Highly-trained clinical liaisons are needed to achieve optimal timing of rehabilitation entry, in turn creating a positive patient experience, effective discharge planning and a reduced risk of readmission. CARF and Joint Commission certifications improve the comprehensiveness of patient treatment and the range of patients a program may treat, as well as help support improved program performance. On average, CARF accredited programs experience a 26% increase in annual patients served as well as a 37% increase in conformance to quality standards.8
Infection Control Specialists
As health systems work to recover from the impacts of COVID-19, it is important for providers to be aware of the infection control protocols that will optimize long-term patient recovery and facility operations. Although infection control standards have always been present in a hospital's operational model, the role they play in patient safety will only grow in importance as health systems work to prevent future outbreaks following COVID-19. A dedicated infection control specialist or team can help a hospital obtain standards such as:
- Certifications set forth by federal programs and agencies to ensure that standards of patient care are consistently met, including areas of quality and safety.
- Appropriate staffing, including physician involvement and nursing expertise, to help ensure that 24/7 care is provided under the guidelines set forth by CMS, as well as additional guidelines established at the facility level to ensure there are personnel fully dedicated to infection control.
- Employee protection protocols to further ensure both patients and hospital staff are taking all of the precautions necessary as the regulations surrounding personal protective equipment (PPE) continue to ramp up throughout the pandemic.
- Patient safety remains a top priority in all inpatient settings. Whether it’s air quality, full-service testing areas or negative pressure isolation rooms, inpatient rehabilitation hospitals are engineered to prioritize patient safety at all times.
- Clinical expertise is a constant presence in an inpatient rehabilitation setting. Research demonstrates that it plays a vital role in rehabilitation efforts for medically complex patients such as those with stroke, brain injury, spinal cord injury or other neurological conditions.
By upholding each of these standards with the help of an infection control specialist or team, a hospital can successfully admit and discharge patients in a safe and healthy care environment no matter their medical complexity.
2. Adapting Through Technology and Innovation

Having access to the latest innovative solutions has allowed providers to not only deliver vital care through equipment or devices, but connect patients and their families separated by distance -even more so now amid ongoing COVID-19 restrictions. For instance, the usage of telehealth technology has rapidly increased since the beginning of COVID-19, with baby boomers accounting for the greatest portion of new users. There has been an overall increase of 155% -jumping from 9% pre-pandemic to 23%.10
Additionally, the increased use of mobile video technology, messaging and image sharing of critical health information in a HIPAA-compliant manner have all become increasingly important as COVID-19 shifts the way care is provided and communication methods are challenged.
By embracing new technologies, rehabilitation programs and their patients can achieve greater levels of success while increasing patient satisfaction, both physically and mentally.
Upgrades to Develop Best-in-Industry Brain Care
Technology is vital to developing leading rehabilitation programs that stand out within the market and deliver the best outcomes. Robotics are among the tools making the biggest impact in the rapidly changing patient population.
For instance, BIONIK lnMotion robots physically guide brain injury patients through tasks by supporting their arms.11 As patients progress, the robots decrease their levels of physical support, thereby adapting to patient capabilities. BIONIK robots are effective for treating patients who have suffered strokes, cerebral palsy, multiple sclerosis, Parkinson's disease and other neurological conditions.
Other emerging technologies that are benefiting medically complex patients include exoskeletons, and even robotics that aid in surgical procedures.
3. Patient and Family Member Experience
In addition to clinical expertise, innovative technology and top-rated rehabilitation programming, support from hospital staff throughout a patient's care journey is just as critical for patient outcomes and family involvement.
The Importance of Follow-Up Calls to Improve Outcomes
Working follow-up calls into standard discharge procedure can produce optimal outcomes for both patients and rehabilitation programs, especially as methods of in-person communication are strained due to the ongoing pandemic. For instance, brain injury patients who receive follow-up calls are more likely to consistently take medication. They are also more likely to attend clinic visits, which correlates with reduced readmission risk.1
Follow-up calls give patients and their caregivers the opportunity to ask questions, resolve any misunderstandings and address any new concerns. Nurses are able to review medications and rehabilitation tasks, repeat instructions, advise on new problems and confirm future appointments.
Supporting the Adult Child Caregiver
For many medically complex patients, an adult child takes on the role of caregiver. Initiatives to support the caregiver can help rehabilitation programs reduce readmissions and improve patient outcomes all while strengthening the relationship between the provider and its patients.
A variety of initiatives can be used to support caregivers:13
- Transitional Support
Training and preparation for the caregiver as the patient transitions from inpatient treatment to at-home care - Educational Materials
Easy-to-understand content that addresses the appropriate phase of the patient’s care journey in addition to potential next steps - Case Managers
Dedicated staff who serve as the caregiver's contact person providing invaluable information on community resources, needed equipment, etc. - Peer Support Groups
A space where caregivers can find emotional support among their peers and learn relevant coping skills - Mobile App Technology
Apps, specially designed for rehabilitation, allow patients and their families to set goals, track progress and share updates. These apps keep patients and caregivers engaged throughout the rehabilitation journey
While a rapidly evolving patient population is challenging, rehabilitation programs can thrive by continuing to adapt their programs to meet the growing demand beyond COVID-19. Developing rehabilitation-specific expertise around these key areas, coupled with a flexible care model that allows a hospital to shift their services to benefit each patient's needs4, can enable rehabilitation programs to reach new levels of success.
Addressing Medically Complex Needs Through Program Optimization
Lifepoint Rehabilitation is one of the largest providers of hospital-based rehabilitation therapy in the country. Lifepoint Rehabilitation’s deep clinical expertise, access to the latest rehabilitation data, innovative technology and quick response to the global pandemic has enabled rehabilitation programs across the country to adapt quickly to the increased patient demand, and reach new levels of clinical and operational success.
References
- Kristen M. Poston. Reducing Readmissions in Stroke patients. American Nurse Today. Dec 2018. https://www. americannursetoday.com/reducing-readmissions-instrokepatients/
- C. Marras, J.C. Beck, et al. Prevalence of Parkinson’s disease across North America. npj Parkinson’s Disease. Jul 2018. https://www.nature.com/articles/s41531-018-0058-0
- Rita Rubin, M. (2020, October 13). As Their Numbers Grow, COVID-19 "Long Haulers" Stump Experts. Retrieved January 18, 2021, from https://jamanetwork.com/journals/jama/ fullarticle/2771111
- A. (2020, September 19). What Now for Rehabilitation Specialists? Coronavirus ... Retrieved January 27, 2021, from https://www.archives-pmr.org/article/S0003-9993(20)30936-9/ fulltext
- Reading, D. (2021, January 16). Beneficial effects of multidisciplinary rehabilitation in post-acute COVID-19 - an observational cohort study. Retrieved January 18, 2021, from https://www.docwirenews.com/abstracts/beneficial-effectsof- multi-disciplinary-rehabilitation-in-post-acute-covid-19-anobservational- cohort-study/
- Getting started in acute care hospitals. Retrieved February 08, 2021, from https://www.asha.org/slp/healthcare/start_acute_ care/#:~:text=Speech%2Dlanguage%20pathologists%20 in%20this,issues%2C%20and%20other%20medical%20 complications
- Amanda Dragga. The Role of Speech-Language Pathologists in Stroke Rehabilitation. Neurorehabilitation. Rhode Island Medical Journal. Dec 2015. http://www.rimed.org/ rimedicaljournal/2015/12/2015-12-20-neuro-dragga.pdf
- CARF International. Accreditation Benefits. http://www.carf.org/ Accreditation/ValueOfAccreditation/Benefits/
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2017). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). https://www.samhsa.gov/data/ sites/default/files/NSDUH-FFR1-2016/NSDUH-FFR1-2016.pdf
- How Covid-19 transformed virtual care preferences, according to our 7,000-patient survey. (2021, January 12). Retrieved January 19, 2021, from https://www. advisory.com/Blog/2021/01/Covid-19-telehealth?utm_ source=member_db&utm_medium=email&utm_ campaign=2021jan19&utm_content=member_ trendingnow_final_blog_x_x_x&elq_cid=4329166&x_ id=0033b00002XWefKAAT
- Keith Shaw. Companies Make Strides in Improving Stroke Rehabilitation With Robots. Feb 2019. Robotics Business Review. https://www.roboticsbusinessreview. com/healthmedical/companies-make-strides-in-improvingstrokerehabilitation- with-robots/
- Jill I Cameron. Supporting Caregivers Across the Care Continuum. University of Toronto: Department of Occupational Science and Occupational Therapy. http://www. gtarehabnetwork.ca/uploads/File/bpd/2017/Concurrent_AM-B_ Caregivers_across_Continuum_Jill_Cameron.pdf

