
Across the nation, communities are experiencing drastic spikes in a variety of behavioral health issues, including anxiety and depression, as people continue to navigate the complexities and stressors brought on by the pandemic. These spikes are extensions of an ongoing crisis in behavioral health globally, and are not expected to decrease once COVID-19 subsides.1
This guide highlights three of the ways strategic joint-venture or contract management partnership can help streamline your hospital’s behavioral health offering to meet the needs of the aging patient population both now and in the future.
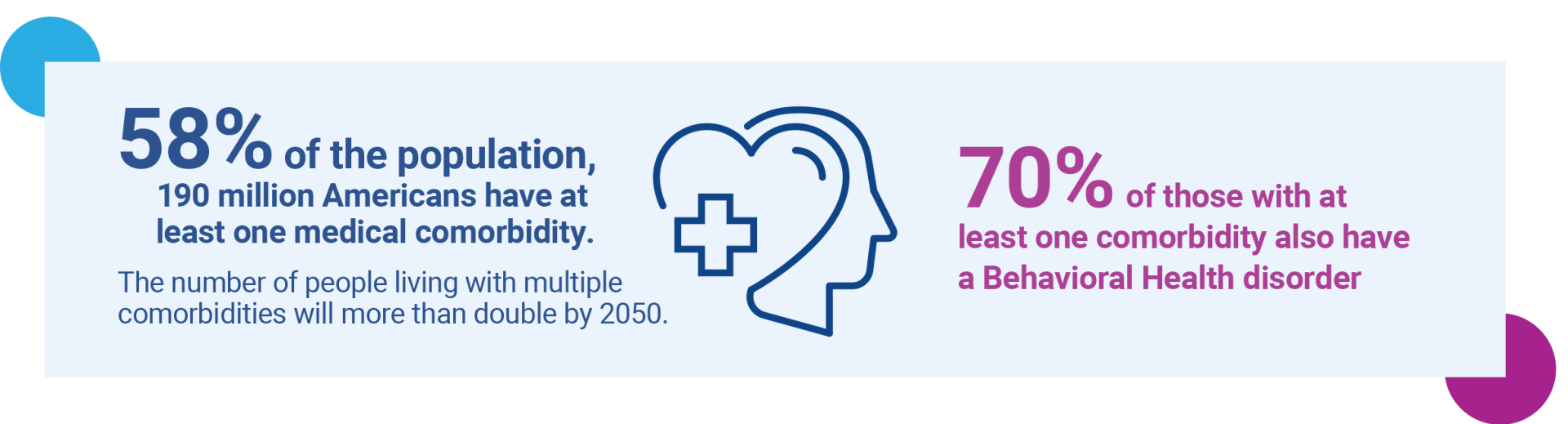
More than 190 million Americans, or 58% of the population, have at least one medical comorbidity, while more than 30 million have three or more. Further, it is expected that people living with multiple comorbidities will more than double by 2050. Of those experiencing at least one comorbidity, nearly 70% also have a behavioral health disorder.2 These statistics highlight the growing need for behavioral health program integration into a hospital’s continuum of care, as many of the patients currently being treated are left undiagnosed. Further, the lack of behavioral health access can hinder a patient’s ability to receive the best care for both their physical and mental needs.
The consequences of not having a dedicated behavioral health program can lead to detrimental losses for a health system, and most importantly, the community it serves – especially as these mental health struggles can lead to overdose, suicide or premature death. Moreover, suicide is the 10th leading cause of death in the U.S. and the second overall cause of death for individuals between the ages of 15 and 24.3
The Current Strain on Health Systems
One in five U.S. adults, or 47.6 million people, experience mental illness each year.4 As of 2017, at least 300 million people across the world were struggling with depression, 284 million with anxiety and more than 178 million with alcohol or drug addiction.1
As these numbers rise year over year, hospitals and health systems continue to be the safety net for behavioral healthcare – especially when community-based services are inadequately resourced. This can cause patients who are experiencing chronic behavioral health disorders to seek care in hospitals not properly suited to provide this type of treatment.5
To efficiently address these issues, health systems are increasing access to this vital treatment through community partnerships, integration of physical and behavioral healthcare in primary care settings, and re-examining the role of emergency departments (EDs) in an effort to alleviate current strains on staff and facility operations as well as reduce care costs.

Research surrounding behavioral health is still emerging, so it can become difficult for hospitals to locate proper education and training for staff members that will help them effectively treat behavioral health disorders. This issue can hinder a hospital’s ability to recommend the most beneficial form of treatment, as they are often unclear about the actions needed to address behavioral health.
Compounding this problem is a workforce without enough psychiatrists, counselors and other clinical staff to fully meet the increasing demand for these services. An analysis from the Kaiser Family Foundation found that the U.S. as a whole was only fulfilling around 44% of its total need for mental healthcare professionals, and an additional 3,300 would be needed to eliminate the shortage.6
Employing highly-trained and educated behavioral health experts, in addition to a dedicated behavioral health department, will help address the growing patient population. Employing these experts also benefits the entire hospital, as behavioral health and rehabilitation collaboration can aid in early identification and treatment of behavioral health needs across all care settings7 – opening the door to patients with physical rehabilitative needs who could benefit from behavioral health services.
However, successful integration of behavioral and physical health services requires cultural shifts. In addition to embedding a psychologist or mental health professional within a medical unit, a hospital must also take into account the necessary collaboration between behavioral health specialists and the rest of the interdisciplinary team of physicians and therapists. This approach has been shown to positively impact those with both physical and mental rehabilitation needs.
Once workforce development concerns are addressed, it opens the door to a more accessible form of care.

In addition to the lack of behavioral health workforce available to serve this growing population, the lack of accessibility to these programs and services continues to take a toll on communities across the country.
In these shortage areas, the ED is utilized as a patient’s primary form of behavioral healthcare, forcing many patients to wait for hours or even days to access an appropriate inpatient psychiatric bed. Research has found that approximately one in eight ED visits involve behavioral health conditions - increasing more than 44% between 2006 and 2017, with suicidal thoughts growing 415%.5,8
Further, this growing strain on EDs hinders their ability to serve patients outside of the behavioral health sector as bed availability continues to be pushed to capacity. As a result, hospitals and health systems are focusing on how to reduce ED overcrowding while connecting these patients with appropriate, timely care.
For areas with greater availability to behavioral health resources, increasing accessibility to this form of care has already produced a variety of benefits. For example, in an effort to reduce acute care utilization, a health system in Tennessee co-located behavioral health professionals in primary care settings to enable real-time consultations. These services included behavioral health screenings and tracking high-need patients for treatment adherence. As a result, the health system reduced ED visits by 68%, hospital care by 37% and overall costs by 22%.5
This has led many providers to examine the specific qualities that could enable their facilities to make these instrumental improvements to their overall performance and outcomes. There is one factor that continues to produce successful results for both a hospital and the community it serves: partnership.

In the past, healthcare consumers typically interacted with the health system only when they were sick or injured; however, a recent Deloitte article has predicted that more health spend will be devoted to sustaining well-being and preventing illness by 2040, while less will be tied to assessing conditions and treating illness. 9 Optimizing a hospital to provide this more comprehensive form of care can present a multitude of challenges if not properly addressed and handled by an industry expert and trusted partner.
Another factor influencing the shift to well-being and prevention treatment is the fact that direct and indirect costs of behavioral illness are estimated to total up to 4% of global Gross Domestic Product (GDP), exceeding the burden of cancer, diabetes and respiratory disease combined. Therefore, if the behavioral health crisis is not adequately addressed, it is projected that the U.S. will experience a $16 trillion negative impact on the global economy from 2020–20301– causing a substantial increase in annual excess healthcare costs and patient lengths of stay in an inpatient setting.6
 Further, health systems have already seen initial financial implications brought on by the pandemic as one recent U.S. study reported the negative behavioral health impacts from COVID-19 rose from 32% to 53% between March and July 2020.1
Further, health systems have already seen initial financial implications brought on by the pandemic as one recent U.S. study reported the negative behavioral health impacts from COVID-19 rose from 32% to 53% between March and July 2020.1
It is also important to understand that as the healthcare landscape evolves to serve this population, the determinant of services provided will shift from the provider to the consumer. This major shift makes it all the more important to stand out in the behavioral health sector – leading many providers to outsource their current or potential behavioral health services to an industry expert to help ensure behavioral health service integration is streamlined with their existing hospital operations.
Benefits of Partnership with Lifepoint Behavioral Health
While the need is great, running a successful behavioral health program is complex and requires specialized expertise that differs from the rest of a hospital’s core competencies. Having a partner with focused behavioral health expertise can benefit hospitals by alleviating the burden of implementing and optimizing a successful behavioral health program. However, one size does not fit all for behavioral health needs. Having a partner that can customize a solution to meet a hospital’s unique needs, while also adjusting to the hospital’s mission and values, is vital for overall program and partnership success.
By addressing these needs, health systems can not only overcome a pressing social challenge, but also improve patient outcomes, reduce costs and create a happier and healthier community.
Lifepoint Behavioral Health, a service line of Lifepoint, is a leader in treating patients with mental health and substance use disorders through partnerships that integrate the latest innovative solutions – producing quality care and superior outcomes.
References
- Judah, R., Allen, S., Rabinowitz, D., Karlinskaya, O., & Piltch, M. (2020). The future of behavioral health: Innovating across sectors to address the global crisis [PDF]. Deloitte Insights.
- Mental health conditions. (2021). Retrieved March 22, 2021, from https://www.nami.org/About-Mental-Illness/Mental-Health- Conditions
- Hannah Ritchie and Max Roser, “Over 800,000 die of suicide and over 350,000 people die from alcohol and illicit drug use disorders annually,” Our World in Data, December 2019. https://www.who. int/teams/mental-health-and-substance-use/suicide-data
- Mental health by the numbers. (2021). Retrieved March 22, 2021, from https://www.nami.org/mhstats#:~:text=20.6%25%20of%20 U.S.%20adults%20experienced,2019%20(13.1%20million%20 people).
- A. (2019, May). Increasing Access to Behavioral Health Care Advances Value for Patients, Providers and Communities. Retrieved March, 2021, from https://www.aha.org/system/files/media/ file/2019/05/aha-trendwatch-behavioral-health-2019.pdf
- Johnson, S., & Meyer, H. Behavioral Health: Fixing a System in Crisis. Retrieved March 10, 2021, from https://www.modernhealthcare.com/reports/behavioral-health/#!/
- N. (2016, September 19). Improving Access to Effective Care for People Who Have Mental Health and Substance Use Disorders: A Vital Direction for Health and Health Care. Retrieved 2021, from https://nam.edu/wp-content/uploads/2016/09/Improving-Accessto-Effective-Care-for-People-Who-Have-Mental-Health-and-Sustance-Use-Disorders.pdf
- Novotney, A. (2018, June). Guarding mental health in the emergency room. Retrieved March 22, 2021, from https://www.apa. org/monitor/2018/06/mental-health-emergency#:~:text=In%20 addition%2C%20a%202017%20report,growing%20by%20 nearly%20415%20percent.
- Forces of change. (2019, March). Retrieved March 10, 2021, from https://www2.deloitte.com/us/en/insights/industry/health-care/forces-of-change-health-care.html

