
The current strain on America’s health system has led many healthcare providers to seek partnership from dedicated experts. This is especially true for rehabilitation. Finding greater expertise and support through a joint-venture or acute rehabilitation management partnership can result in significant quality improvement, cost savings and high-demand service line optimization. While the healthcare landscape has never been more challenging, this is a time of great opportunity
This article outlines how rehab partners can support healthcare providers, the key qualities to look for in a partner and the top questions to ask a potential partner.
The Advantages of Support from an Acute Rehab Partner
Healthcare executives find partnerships preferable for a few key reasons, according to a survey by Deloitte.1
These reasons include:
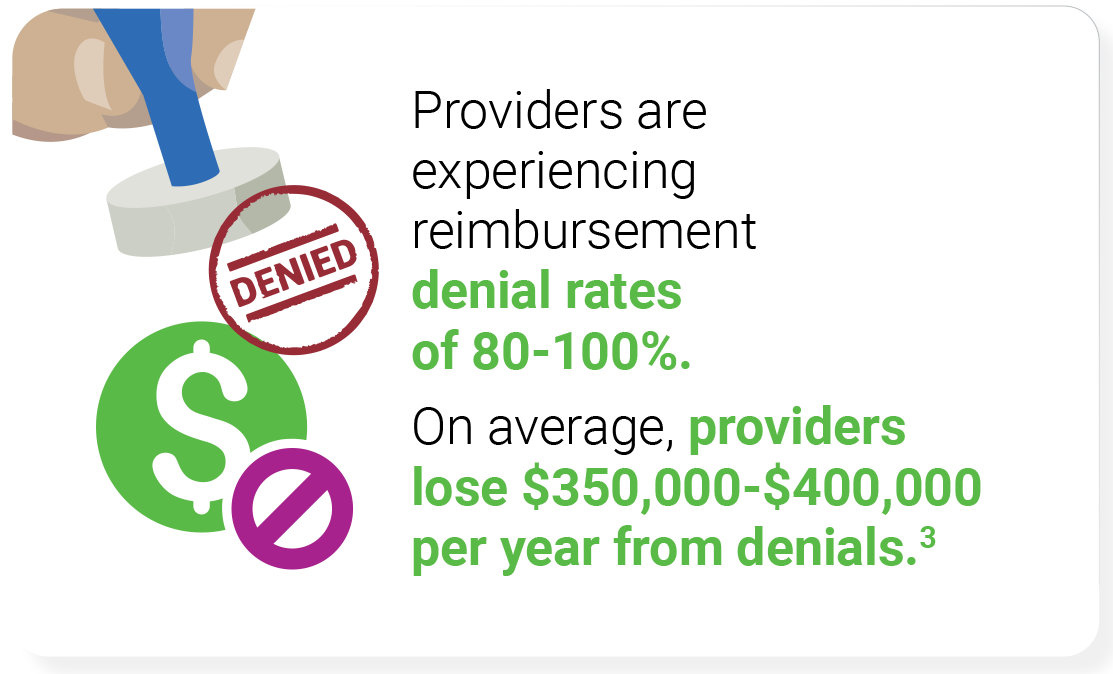
- Lower post-acute expenditures. The most effective partners can improve financial throughput and improve cash on hand by reducing several critical cost factors, including emergency room visits, lengths of stay, readmissions and claim denials.
- Enhanced overall performance with fewer in-house resources. Partners are able to share the responsibility for program infrastructure, allowing providers to maximize their program value and minimize up-front costs.
- Increased patient access and improved employee retention.
- Greater scale and speed to market. Partners have national rehab data and resources to ensure providers are able to quickly adapt and meet growing demands, such as what we’ve seen from the COVID-19 pandemic and changes in patient population.
In a survey of healthcare executives, partnership was preferred over solely owned post-acute providers.1
Reasons included:
- Improved patient experience
- Reduced capital expenditure
- Scalability
- Speed to market
- Ability to focus on core competencies
Top 5 Qualities That Make a Great Acute Rehab Partner
While the benefits are clear, not all joint-venture or acute rehab management partners are created equal. When evaluating a potential partner, the following five qualities are key indicators of long-term success.
- Clinical and Quality Effectiveness
Providers should look for partners who have experience helping programs achieve top quality certifications, such as the Commission on Accreditation of Rehabilitation Facilities (CARF) and The Joint Commission. Partners must be able to demonstrate clinical effectiveness with reduced readmission rates and better patient outcomes. Achieving high standards, like CARF, also helps your program stand out from others and can increase annual patients served by 26%.2 - Proven Track Record in Quickly Adapting to Industry Challenges and Optimizing Performance Based on Need
Suitable partners have already achieved impressive results for other healthcare providers, including helping them rebound faster than the industry from COVID-19. Having access to national rehab data and best practices while also having the flexibility to quickly adapt programs based on changes to the environment further strengthens an already proven track record. - Robust Network of Medical Directors
Rehab programs are already being impacted by the growing talent shortage. Strong medical directors are a key component to any successful program, but are hard to identify and retain. Partners must have a strong network of medical directors who are focused on provider engagement. - Patient Throughput Management
An effective partner should have a well-organized system for efficiently moving patients through phases of care. Careful management ensures that patients enter rehab at the right time in their care journey and stay for the appropriate amount of time. Achieving this reduces readmission rates, lowers per-patient costs and increases patient satisfaction. - Expert Regulatory and Compliance Team
The current changing regulatory environment makes it challenging to assure compliance. An ideal partner will be up to the task with a highly competent regulatory and compliance team who specializes in rehab. They should be able to keep abreast of the latest changes and prepare for regulation expansions, navigating the system’s intricacies to reduce denials.
Find Your Ideal Rehab Partner
Receiving support from a third-party team of rehab experts enables healthcare providers to reach the highest levels of performance in this niche and highly-regulated space. This allows them to best serve patients recovering from COVID-19, optimize hospital operations and efficiency, and improve overall patient satisfaction and care quality. Lifepoint Rehabilitation serves over 150 hospital-based rehab programs, optimizing program features ranging from infection control and clinical best practices around COVID-19, to staffing and appeals. Their accomplishments include successful appeal of 90% of all claims they manage, as well as a 99% reduction of management vacancies.
Finding the Right Partner: Key Questions to Ask
Further assess the quality of a potential partner by asking targeted questions:
How are you able to quickly adapt to the changing healthcare environment?
They should have access ti national rehab data from hospitals and hold a proven track record of helping partners succeed through times of adversity, all while continuing to provide clinical and operational excellence.
What are your quality metrics?
A partner that gets results has an evaluation system that goes beyond the minimal government requirements and that assesses the most important performance benchmarks, such as changes in FIM and PEM, and discharge-to-community rates.
What do you do to decrease patient readmission risks?
To effectively minimize readmissions, candidates should have a clear and proven system for maximizing patient readiness for discharge.
How do you drive clinical efficiency?
Their answer should list practical actions that have a measurable effect on clinical efficiency.
What is your denial rate?
Denials add up to significant expenses for providers. Ideal partners utilize thorough compliance and a successful claim appeal process to obtain a low denial rate.
Do you utilize technology that can flag regulatory issues before they become larger problems?
Implementing flagging software can minimize resources devoted to resolving regulatory problems.
How do you promote patient advocacy and improve access to care?
Highly-trained clinical liaisons should be prominent figures in partner plans for enhancing both patient access and engagement. Additionally, the right partner will implement the latest best practices to ensure patients in need of inpatient rehab receive care in a safe environment.
How do you promote provider retention and engagement?
Optimizing retention is critical, as close to half of disengaged employees plan to leave their jobs within a year. Partners should place special focus on training and career development opportunities where hospital employees report lowest satisfaction rates. To combat the critical provider shortage, partners should have access to a strong network of physicians, therapists and nurses.
Do you utilize technology for improving both provider and patient engagement?
The latest technologies should be used to enhance engagement among physicians, therapists and the patients themselves. Additionally, tech solutions should be leveraged to enhance communication between patients and family members, especially when family is separated by distance or visitor restrictions.
References
- Viewing post-acute care in a new light: Strategies to drive value. Deloitte Center for Health Solutions. 2017. https:// www2.deloitte.com/content/dam/Deloitte/us/Documents/ life-sciences-health-care/us-lshc-post-acute-care-innovationreport.pdf
- CARF International. Accreditation Benefits. http://www.carf. org/Accreditation/ValueOfAccreditation/Benefits/
- Lowe GS. How Employee Engagement Matters for Hospital Performance. Healthcare quarterly (Toronto, Ont.) 2012 Apr;15(2):29-39. doi:10.12927/hcq.2012.22915.

