 In order to effectively treat the 47.6 million individuals experiencing mental illness each year,1 hospitals must first identify one of the key contributors – location. Community-based and urban communities experience unique challenges that often create substantial obstacles for hospitals to provide, and community members to receive, proper behavioral health treatment.
In order to effectively treat the 47.6 million individuals experiencing mental illness each year,1 hospitals must first identify one of the key contributors – location. Community-based and urban communities experience unique challenges that often create substantial obstacles for hospitals to provide, and community members to receive, proper behavioral health treatment.
As the nation begins to prioritize mental and behavioral health, hospitals are looking for strategies to meet that need. Read this guide to discover the unique challenges and opportunities that come with behavioral health in urban and local – also referred to as community-based – locations and how hospital leaders can improve the overall health of their community by expanding access to these services.
 Behavioral Health Challenges Within Local Communities
Behavioral Health Challenges Within Local Communities
Although medical and behavioral health issues affect individuals across the nation, access to care is not equally distributed. About one-fifth of the U.S. population lives in community-based counties, and one-fifth of those, or about 6.5 million individuals, have a mental illness.2
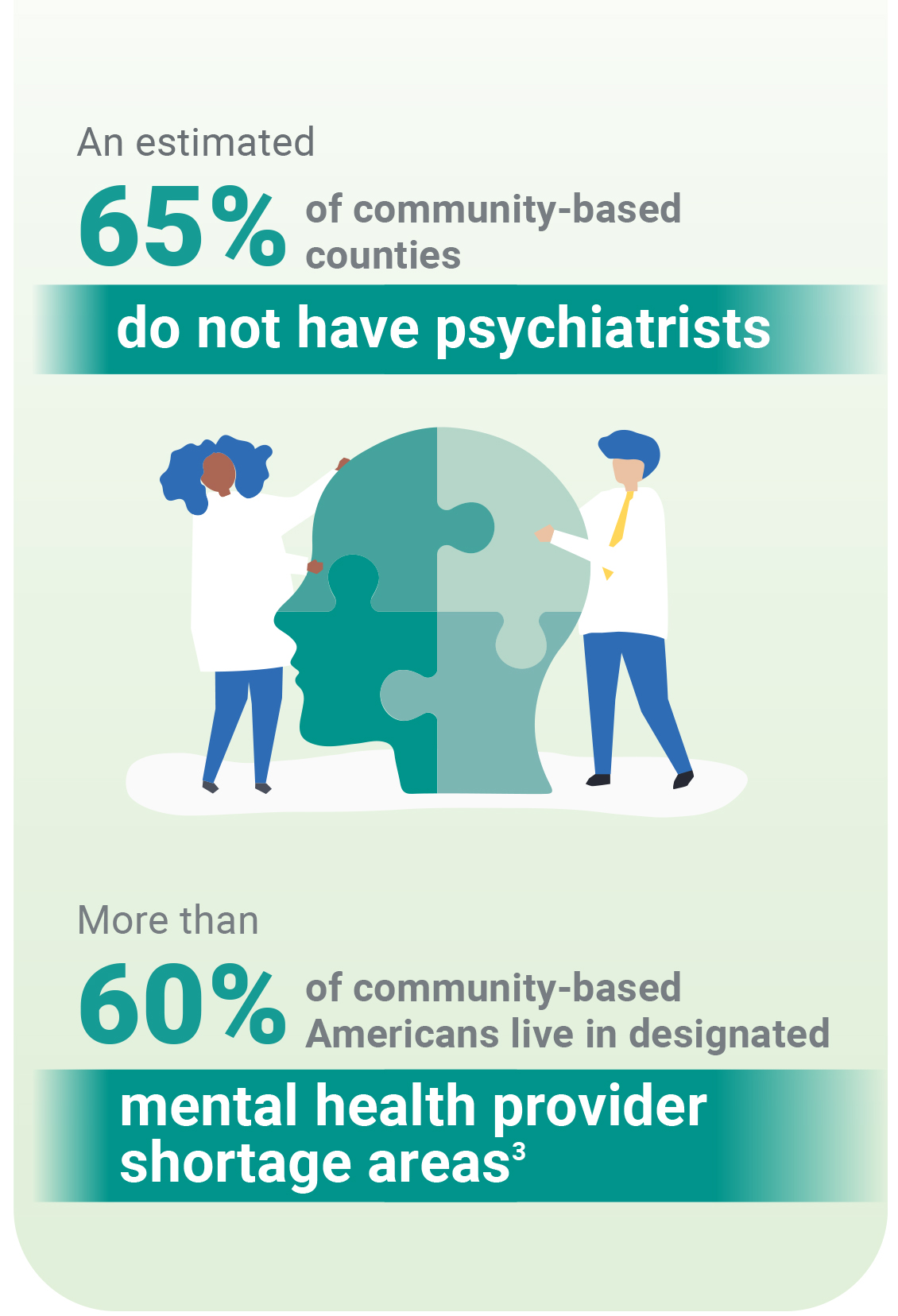
It is estimated that as many as 65% of community-based counties do not have psychiatrists, and more than 60% of community-based Americans live in designated mental health provider shortage areas.2 Between 2010 and 2019, these hospitals faced increased risks of closure - a risk that will continue unless appropriate access to care and staffing issues are addressed.3
Additional obstacles restricting these communities from obtaining proper behavioral health treatment include:
- Socioeconomic Factors: This includes higher unemployment rates and greater numbers of individuals living below the poverty line. Even if an individual or family is employed, receiving insurance benefits for mental healthcare is a rarity.
- Public Acceptance: The negative stigma surrounding behavioral health treatment in some communities continues to affect an individual's willingness to receive care. A higher sense of isolation and lower education rates can also limit a family or an individual's understanding of the benefits of behavioral health and the crucial purpose it serves for overall population health.2,4
- Delayed Public Understanding: Lower education rates, coupled with restricted access to behavioral health resources, can often limit a person's ability to recognize signs of mental illness and understand their care options. This leads to delayed diagnosis and care, increased illness severity and, ultimately, higher care costs.5
Although these are deeply rooted challenges, opportunities to combat them are available to health systems that want to improve behavioral health access in their communities.
Steps to Improve Community-Based Access
Discussions around the integration of mental health into primary care settings within local communities date back to the early 1970s. However, years of re-education, along with drastic spikes brought on by the pandemic, have led to a renewed interest in and policy support for efforts to strengthen behavioral health integration.5
Tools that have yielded positive results in addressing issues around staffing shortages and education, as well as the quality of behavioral healthcare offered, include:5
- Development and implementation of electronic medical records (EMRs) to support clinical integration and communication;
- Continued integration of educational resources and programs emphasizing the importance of behavioral health treatment in an effort to further combat the negative stigma around receiving care;
- Expanded use of technology, such as telehealth, to provide psychiatric support among other treatment options; and
- Support from an experienced partner who is dedicated to providing high-quality, tailored behavioral healthcare to benefit a community's specific needs.
Through these tools, health systems can help combat negative stigma surrounding treatment, provide valuable resources for mental and behavioral health education and ultimately help ensure this vital form of care is easily accessible no matter the location.
Similar to local community challenges, the urban demographic has its own hurdles to overcome in order to properly address the issue of behavioral health access.

Urban Community Obstacles
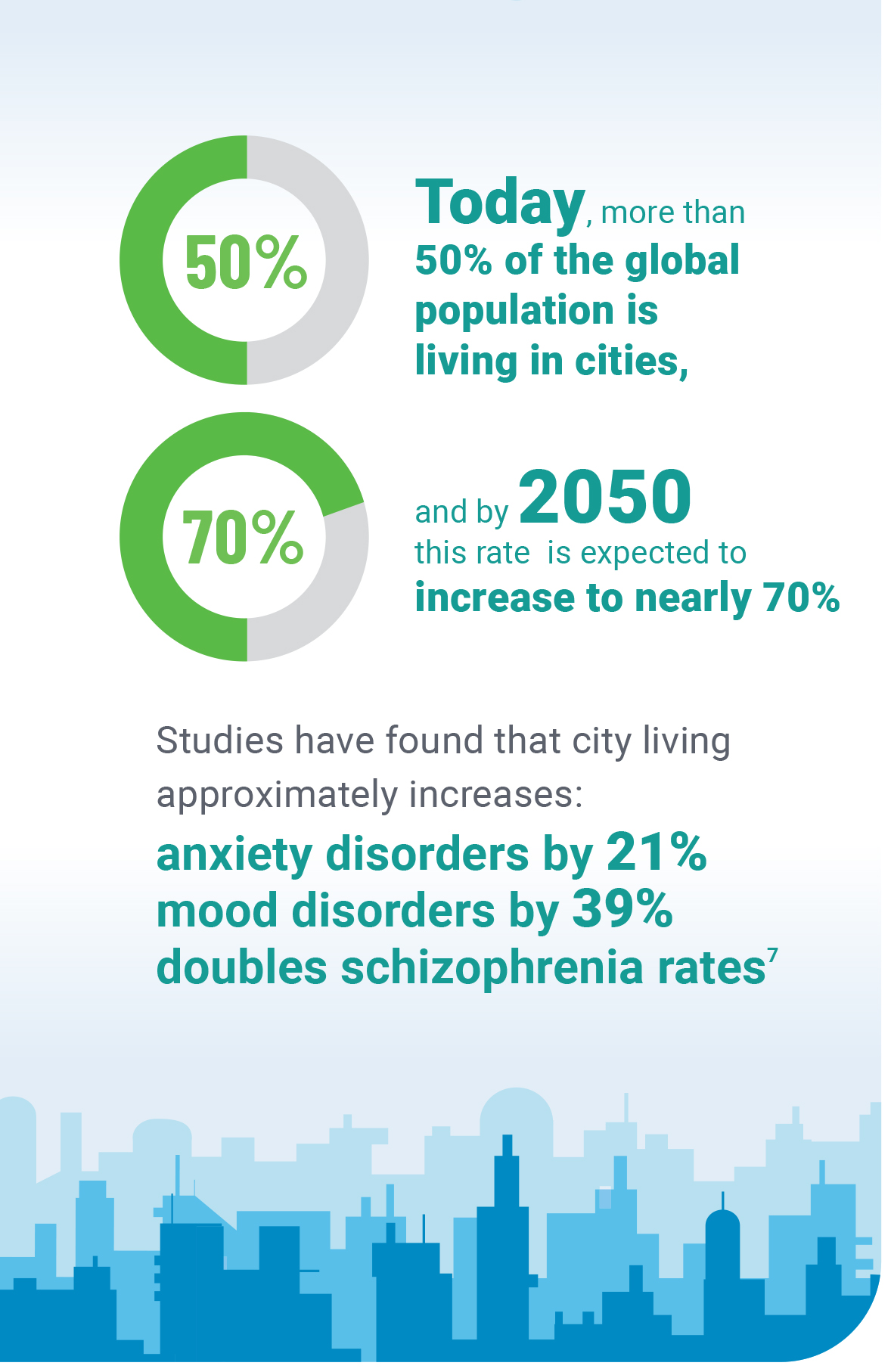
Today, more than 50% of the global population is living in cities, and by 2050 this rate is expected to increase to nearly 70%.6 However, as more individuals migrate to urban communities, the risk of developing a mental or behavioral health illness rises. This has been found in studies that highlight city living increases anxiety disorders by approximately 21%, mood disorders by 39%, and roughly doubles schizophrenia rates.7
Additionally, where local communities experience physical distance as an obstacle when seeking behavioral health treatment, urban communities run the risk of overpopulation. This leads to crowded emergency departments (EDs) and mental health treatment centers - impeding an individual's ability to receive high-quality services. These densely-populated areas are known for elevating risk factors associated with mental illness due to poverty, homelessness, physical and mental disabilities, drug and alcohol abuse, and social alienation - factors that have only increased since the onset of the pandemic.7
Although urban areas maintain a reputation of greater access to services and resources, disadvantaged individuals still struggle to obtain care due to financial and transportation limitations and the disproportionate availability of behavioral health resources in various neighborhoods. This can lead to a self-reinforcing cycle, called social drift, where certain areas with higher rates of poverty and mental illness produce greater social disorder and crime which further increases mental illness risk. However, there is a solution.
Urban Area Opportunities
Although the factors limiting behavioral health treatment in urban communities differ from community-based areas, the need for these vital services remains. By utilizing existing services and elevating them to help ensure they are easily accessible to every individual in every neighborhood, hospitals can address the many challenges within urban landscapes.
Steps to improve access and education for behavioral healthcare include:
- Understanding neighborhood demographics. A collection of factors can greatly impact a neighborhood's ability to access critical behavioral healthcare. Identifying areas within urban neighborhoods that are underserved and prioritizing the integration of care options, in addition to increasing education and awareness, can offer substantial benefits within these communities.
- Providing quality resources. Prioritizing staff training and education around behavioral health, in addition to hiring qualified psychologists and therapists, will not only aid in combating ED overcrowding, but will also help reduce the possibility of readmission following treatment.
- Behavioral Health education. The lack of behavioral health education, coupled with negative stigma around receiving treatment, has led individuals to delay care, and not fully understand the signs and symptoms of mental illness. Integrating behavioral health programming into a primary care setting can help introduce the benefits of this treatment to a larger community base, therefore reducing stigma and opening the door to potential co-location of healthcare services.
By understanding the unique obstacles presented in both community settings, hospitals can identify proven strategies to meet the challenges. However, many hospitals today struggle to successfully integrate a behavioral health service line independently due to the specialization required, lack of proper education and resources - leading many to outsource to a trusted partner.
Advantages of Behavioral Health Partnership
The challenges presented in both communities are clear; however, the resources available to aid in behavioral health prevention, treatment and recovery are often difficult for health systems to achieve without the specialized support of an industry expert.
Behavioral health experts understand the specific challenges hindering accessibility and are well-equipped to handle the obstacles through the integration of a flexible strategy designed to address the unique needs of the community. Being able to rely on a behavioral health expert for high-quality programs and services, fully trained and educated clinical staff and access to a national database of resource material, helps to alleviate the burden of independently running a successful behavioral health hospital.
Lifepoint Behavioral Health serves as a leader in treating patients with mental health and substance use disorders. Our partnership models allow us to integrate the latest innovative solutions and expertise to produce quality care and outcomes no matter location.
References
- Mental health by the numbers. (2021). Retrieved March 22, 2021, from https://www.nami.org/ mhstats#:-:text 20 .6% 25 % 20of%20U .S. %20adults% 20 = experienced, 2019% 20( 13 .1 % 20million % 20people).
- Morales, D. A., Barksdale, C. L., & Beckel-Mitchener, A. C. (2020, May 4 ). A call to action to address rural mental health disparities. Journal of clinical and translational science. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC7681156/.
- Summers-Gabr, N. (2020, May). Rural-Urban Mental Health Disparities in the United States During COVID-19. American Psychological Association. https://psycnet.apa. org/fulltext/2020-38395-00 l .pdf
- Gale, J., Janis, J., Coburn, A., & Rochford, H. (2019, December). Behavioral Health in Rural America: Challenges and Opportunities. Rural Policy Research Institute. https://rupri.org/wp-conten t/up loads/Behaviora 1-Health-inRural- America-Challenges-and-Opportunities-ExecutiveSummary-.pdf
- Gale, J. A., & Lambert, D. (2006,January 1). Mental Healthcare in Rural Communities: The Once and Future Role of Primary Care. North Carolina Medical Journal. https:// www. ncmed ica I journa l.com/content/6 7 /1 /66.
- Gruebner, 0., Rapp, M. A., Adli, M., Kluge, U., Galea, S., &; Heinz, A. (2017, February 24 ). Cities and Mental Health. Deutsches Arzteblatt international. https://www.ncbi.nlm. nih.gov/pmc/articles/PMC53 7 4 256/.
- Litman, T. (2021, March). Urban Sanity Understanding Urban Mental Health Impacts and How to Create Saner, Happier Cities. Victoria Transport Policy Institute. https:// www.vtpi.org/urban-sanity.pdf

