
Denials for Medicare and private insurance claims are steadily increasing, becoming a critical concern for healthcare providers across the spectrum. In fact, both commercial and public payers are now denying about one in every 10 submitted claims, costing health systems up to 2% of net patient revenue, according to the Advisory Board.1
Learn the key factors causing a rise in denials for healthcare providers and proven strategies to help patients receive the medically-appropriate care they need to reach a full recovery in this Q&A with Appeals and Denials expert Emily Morgan, JD, SLP, from Lifepoint Health.
1. What trends over the past few years have impacted denials?
- In the past, denials were prevalent among orthopedic admissions. Recently denials have shifted to shorter stays and the 40% admissions, especially for nonsurgical admissions, such as pelvic fractures, UTI, GI and metabolic diagnoses.
- Denials have become increasingly more universal, rather than regional, although each Medicare Administrative Contractor (MAC), which is a regional contractor, may focus on a different aspect to monitor within their territory.
2. How is the Medicare denials system set up across the nation?
- The Centers for Medicare and Medicaid Services (CMS) requires MACs to monitor their own disbursements, generating MAC-initiated denial reviews.
- The U.S. Department of Health and Human Services (HHS) authorizes reviews by the Office of the Inspector General (OIG) for both Managed Care and Medicare claims. The OIG may elect to review claims for perceived over-utilization or reporting discrepancies, as well as a continuum of services including acute care hospitals, inpatient rehabilitation hospitals, skilled nursing facilities, home health agencies and outpatient physical therapy providers.
- Through computer data analysis, CMS reviewers readily watch for trends and errors and target sites that may have billing patterns that stand out from their regional or national peer groups.
3. What additional types of CMS audits and reviews are occurring?
- CMS’s Targeted Probe and Educate (TPE) program involves prepay audits intended to assist providers in reducing denials and appeals.
- Supplemental Medical Review Contractors (SMRC) conduct medical reviews of Medicare claims nationwide and focus on coverage, coding, payment and billing compliance.
4. What trends should the industry continue to expect for claim denials?
- Regulatory requirements must be met to ensure that Medicare funds are spent appropriately. However, denied claims may very well trend down as sites improve their ability to document supporting medical necessity.
5. What tools can be put into place to limit denials?
- A structured support plan provided by a knowledgeable and experienced team of appeals specialists will help limit denials. Due to the complexity and specialization often required, many health systems are finding success through focused support from a dedicated rehabilitation partner that has proven expertise in limiting denials.
6. What members of the acute rehabilitation team should be involved in appeals?
- Since the patient journey begins in an acute care setting, it is crucial for the interdisciplinary rehabilitation team to collaborate with the full range of acute medical specialists to understand how each clinician’s documentation supports medical necessity. Ensuring consistent and appropriate documentation across each stage of the care continuum is more important than ever before.
7. Why do facilities receive denials for rehabilitation claims, sometimes after the patient has received services?
- In order to ensure compliance with regulatory requirements as well as reduce fraud and abuse, CMS is obligated to monitor appropriateness of billing, documentation and medical necessity. At times, the CMS review is conducted after a patient has already been discharged from care services.
- Managed Medicare also conducts regional reviews for risk analysis of care provided to their enrollees as a trend analysis.
8. What is extrapolation?
- When extrapolation is appropriate, the auditor will check a small, random, statistically valid sample of claims and will use that small sample to determine the “error rate.” The error rate is then applied to the universe of claims, which is usually a period of three years. For example, if the error rate in a small sample of 30 claims is 25%, then it is assumed that there was an error rate of 25% of all claims submitted in the three-year period and an overpayment is calculated accordingly.
- Extrapolation is used when certain audits find a sustained, or high level of payment error, and records are too large for individual review. Further, extrapolation may be used after documented educational interventions, such as a TPE program as described above, have failed to correct payment errors.
9. How does Lifepoint Rehabilitation constantly monitor and learn from denials trends nationwide?
- Lifepoint operators are given timely feedback about the nature of current audits and their status.
- Lifepoint’s national presence enables it to see the broad picture of how different MACs are responding. This allows for better understanding of national trends in the SMRC and Recovery Audit Contractor (RAC) reviews as reasons for denial.
- Lifepoint’s comprehensive analysis demonstrates how denials are trending over time so it can be quickly determined if updates are required across all managed acute rehabilitation programs.
How do Lifepoint’s denial rates compare to the industry average?
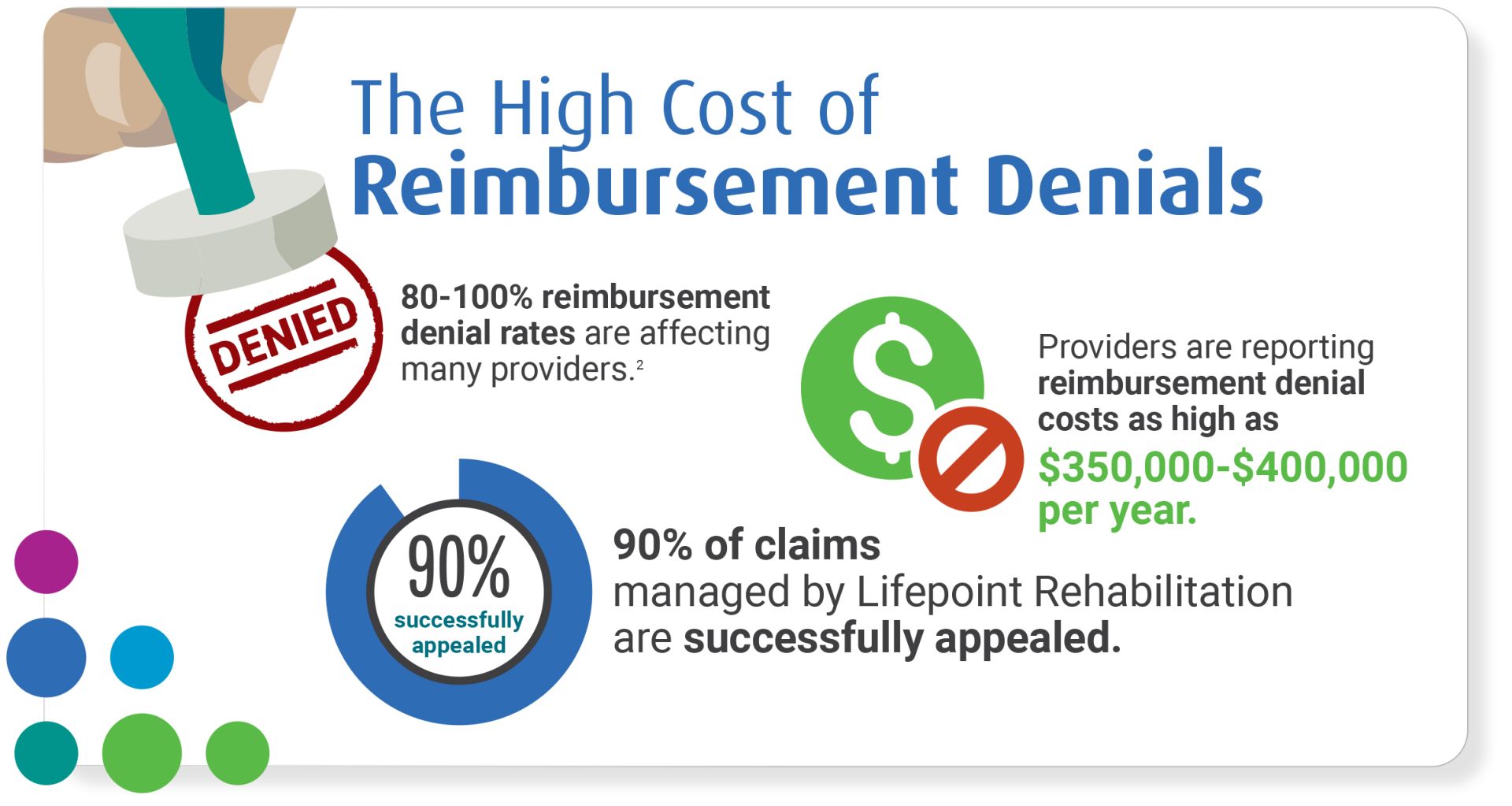
- Lifepoint has a history of outperforming the industry average for overturning claims that have been denied at all levels of appeal, reducing the financial impact to those providers.
- Currently, Lifepoint has a number of pre- and post-payment reviews that were found to be 100% favorable with no denials at the Alternative Dispute Resolution (ADR) level.
Overcoming Denial Challenges Through Partnership
A partnership to help overcome denial challenges can be impactful, as this trend is expected to rise in the coming years. Now more than ever, having a dedicated rehabilitation partner that can reduce the burden of running acute rehabilitation can help overcome these key challenges and enable your facility to focus on what matters most: the patient.
About Our Appeals Team
Lifepoint’s dedicated denial and appeals team continues to efficiently and successfully navigate the ever-changing denials landscape, in turn reducing denial rates and opening the door to a larger patient population in need of vital care. Within that team, Director of Appeals Emily Morgan provides a depth of expertise, having been with Lifepoint Rehabilitation since 2008 with a specific focus on acute rehabilitation denials. Emily has also worked on skilled nursing facility (SNF), home health (HH), acute hospital, long-term acute care (LTAC) hospital, and physician appeals for more than 25 years.
References:
- Revenue Cycle Advancement Center’s 2017 Hospital Revenue Cycle Benchmarks, Advisory Board
- Youngstrom N, B Anholzer. IRF Claim Denials Are Mounting; Auditors Use Coverage Guidelines, Eye Physician Notes. Report on Medicare Compliance. 2017 Sept;26:1-3. https://www.hcca-info.org/Portals/0/PDFs/Resources/Rpt_Medicare/2017/rmc092517.pdf?ver=2017-09-22-104822-433

